Background
In 1997, the U.S. Congress passed a law called "The Food and Drug Administration Modernization Act of 1997". The aim was to improve the authorization process to market medical devices, that is to say somehow alleviate the process to promote patient access to new technologies while respecting safety standards [1]. Concretely, the FDA considers alternatives to randomized clinical trial [2,3] in particular testing protocols using as control groups non-competing groups such as historical controls (e.g. literature, patient records ) as objective performance criteria (OPC).
For some investigational medical devices (e.g. replacement heart valves, carotid stents), the US Food and Drug Administration (FDA) has allowed the approval process to include single arm clinical studies, and the control group has been replaced by expected standard results known as “objective performance criteria” (OPC) without compromising the scientific integrity required by its mission of public health safety [4,5,6,7,8,9].
The OPC is a criteria derived from published literature and/or other sources of reliable data or registries. It is used as a comparator in single arms trials where randomization is impractical or impossible. It should reflect the current level of care and should be updated periodically.
Conducting a double-blind randomized controlled trial (RCT) to demonstrate the efficacy of Acupuncture against placebo is challenging. If acupuncture needles are considered as a medical device, the methodology OPC (Objective Performance Criteria) used by the FDA for some medical devices approval could be used as a valid scientific alternative to show efficacy of Acupuncture.
In 2011, this concept of OPC was proposed by TN Brignol and P. Verta as an alternative methodology for Acupuncture clinical trials, at ICMART XIII World Congress (International Council of Medical Acupuncture and Related Technique) [10].
An article explaining this concept was published in 2011 in the French Journal “Acupuncture & Moxibustion” [11].
Over the last decade, complementary and alternative medicine (CAM) has been widely used in maternity practice all over the world. Women from different cultural backgrounds prefer the use of specific CAM modalities. Maternal consideration of fetal in addition to personal well-being play an important role in approaches to maternal medical care. According to studies from Germany and Sweden, acupuncture use among obstetric (OB) patients rates in the 4% to 13% range [12, 13].
In this paper, we present a brief introduction to the use of OPC (Objective Performance Criteria) as an alternative to double-blind RCTs. Then we report the application of the OPC concept in two clinical trials performed in 2011 and 2012 by midwives for obtaining the Obstetric Acupuncture Diploma from the University of Lille 2, France [14, 15].
Application of OPC in Acupuncture clinical trial on perineal relaxation during fetal expulsion
In France, since 2009, the practice of acupuncture by midwives is legal provided that they hold the Diploma of Obstetric Acupuncture delivered by Universities in France.
- Patients and Method
In 2011, two midwives from Jeanne de Flandre Hospital in Lille (France) used the OPC methodology for evaluating the effects of SP6 (sanyinjiao) puncture on perineal relaxation during fetal expulsion.
Fifty-four primiparous (para 1) or biparous (para 2) pregnant women participated in the trial. The inclusion criteria were: a scarred uterus (those who underwent a cesarean section during their first pregnancy and had not given birth through the vagina), vertex presentation, and with a gestational period ≥ 37 weeks (gestational age calculated from the first day of the mother’s last menstrual period). The exclusion criteria included: multiple pregnancies (twins or triples), breech presentation, gestational period < 37 weeks, multiparous women. The efficacy endpoint was the perineal tears caused by the vaginal delivery.
The needles were inserted bilaterally at SP6 (sanyinjiao), when the cervix was in complete dilation, or immediately or within a few minutes, even just before the expulsive efforts.
2. Results
The results were compared with data from a reliable registry that served as a substitute to the traditional control group. It was the 2010 database (DB 10) of “Jeanne de Flandre Hospital” in Lille (France), collecting data about the same population than the study: para 1 and para 2 women with previous caesarean section (n = 2,216 patients).
For a high birth weight greater than 3,500 g (about 7.71 £), known to be a high risk factor for perineal tears during vaginal delivery, in DB 10, only 37.4% of patients have preserved an intact perineum after delivery (vs 48% in the Acupuncture Group of the study). No complex perineal tear in the Acupuncture Group was found (vs 4.20% in DB 10). In the Acupuncture Group, there were 16% of simple tear vs 35.2% in DB 10. On the other side, episiotomies were higher in the acupuncture group than DB 10 (36% vs 23.2%). (Figure 1).
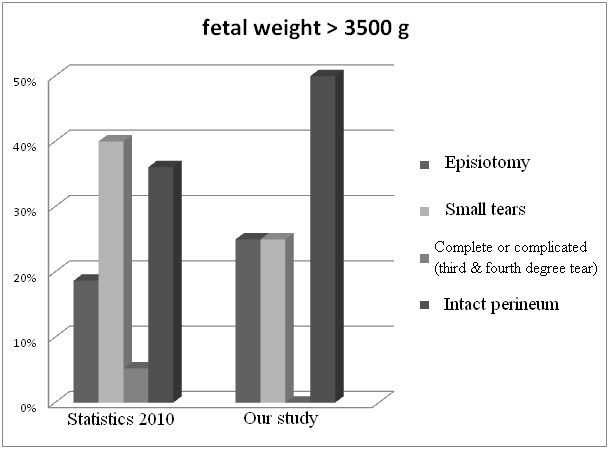
Figure 1. Assessment of the perineum according to fetal weight.
Another risk factor for perineal tears is an infant’s head circumference greater or equal to 35cm (about 13.78 inch). More than half (58.33%) women who gave birth to a baby with head circumference greater than 35 cm have preserved an intact perineum after childbirth in the acupuncture group (vs 44.55% in the DB10 group). (Figure 2). On the other side, episiotomies in the acupuncture group were higher than DB 10 (36% vs 23.2%). (Figure 1).
A bias may exist concerning a higher frequency of episiotomy in the acupuncture group. In the acupuncture group of 54 patients, there were 29 patients without instrumental delivery, 21 patients requiring instrument assisted delivery and 4 patients were excluded from the study due to caesarean section at the end of the labor. The use of forceps, vacuum extractor or a combination of both was respectively 38.1%, 44.28%, and 19%. These cases of instrumental birth generated a significant percentage of episiotomy, respectively 87%, 56% and 50%. But percentages and types of instrumental delivery in BD10 were unknown, less instrumental delivery could explain the higher number of episiotomy in our trial.
However, the difference was more significant if only childbirth from primiparous was considered: 47% of intact perineum in BD10 versus 72% in the acupuncture group.
These results showed that acupuncture has sufficiently relaxed the perineum to prevent severe perineal tears.
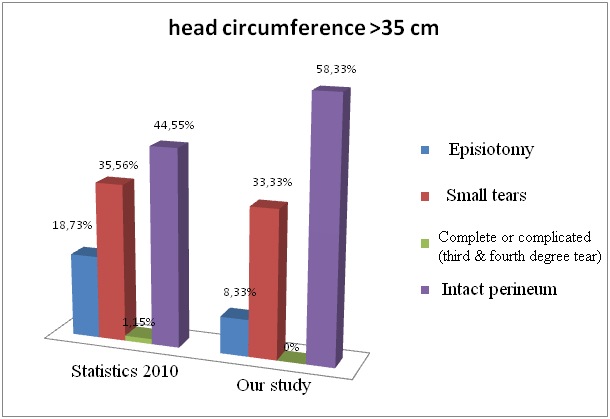
Figure 2. Assessment of the perineum according to infant’s head circumference.
- Limitations of the study
The study was not randomized; therefore known and unknown bias could have influenced results.
Application of OPC in Acupuncture clinical trial on the third stage of labor
The trial was conducted by two midwives at Paul Gellé Hospital Maternity (Roubaix, France) from October 1, 2012 to January 31, 2013.
1. Background
The third stage of labor starts from the birth of the infant to delivery of the placenta and membranes. It is composed of three phases: placenta separation, placenta descent, placenta expulsion. If the placenta fails to be expelled within half an hour after delivery of the infant, the condition is called retained placenta. A prolonged third stage of labor is considered to be a risk factor for postpartum hemorrhage.
The postpartum hemorrhage is a serious complication of childbirth that may involve life-threatening to the mother (first cause of maternal death). To prevent this issue, 5 IU oxytocin is injected in a systematic manner, even for patients without particular risk. Few studies exist in the literature about the effect of acupuncture on delivery of the placenta [16, 17, 18].
The two midwives contacted a dozen maternity hospitals in France (Strasbourg, Rouen, Lille, Brest, Paris, Lens, etc.), but also in Canada. After telephone conversation with midwives of these hospitals, they learned that acupuncture is not or is rarely used for the third stage of labor. The reasons were lack of time and trouble to choose the most suitable points.
- Patients and Method
In this OPC type study, the two points SP6 (sanyinjiao) and KD16 (huangshu) were selected. They were punctured as soon as possible after cord clamping.
Twenty nine pregnant women were included. The endpoints of the study are: time between infant birth and placenta expulsion; decrease of bleeding, decrease of postpartum hemorrhage, number of artificial delivery of the placenta.
The endpoints were compared with the standard norm derived from published clinical trial results, and reviewed by the Cochrane Collaboration [19], serving as a substitute to the traditional control group.
3. Results
a. Delay between the birth of the infant and delivery of the placenta
In spontaneous delivery of the placenta, the time is estimated less than 10 minutes. This value is the same in the OPC trial as the one found in the Cochrane Database 2001, revised in 2004 [19]. According to the literature, it is necessary to act if the delivery did not take place after 30 minutes. In this sample of patients who benefited from the acupunctural method, the longest delivery is 13 minutes, with an average time of 7min 23sec. There is no statistically significant difference between the delivery promoted by acupuncture and the delivery promoted by oxytocin (χ2 test, p> 0.05). Therefore the use of acupuncture is as effective as pharmacologic method to reduce the length of the third stage of labor.
b. Amount of blood loss and number of postpartum hemorrhage
The Cochrane Collaboration in 2004 and updated in October 2009 (seven RCTs, n> 3,000) [19] indicates fewer postpartum hemorrhage (clinically characterized by a amount of blood loss equal to or greater than 500 ml) when oxytocin is used in preventive measure (relative risk (RR) for blood loss greater than 500 ml = 0.50; confidence interval (95% CI = 0.43 to 0.59) compared to no treatment. Furthermore, the average amount of blood loss in this OPC trial was 374 ml versus 548 ml in the control group reported by the Cochrane Collaboration. In this sample of 29 patients, the average amount of blood loss in immediate postnatal is 210 ml. One patient presented a hemorrhage with blood loss estimated to 550 ml. (Figure 3).
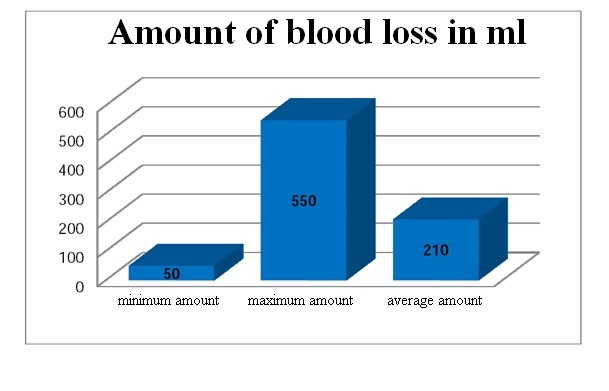
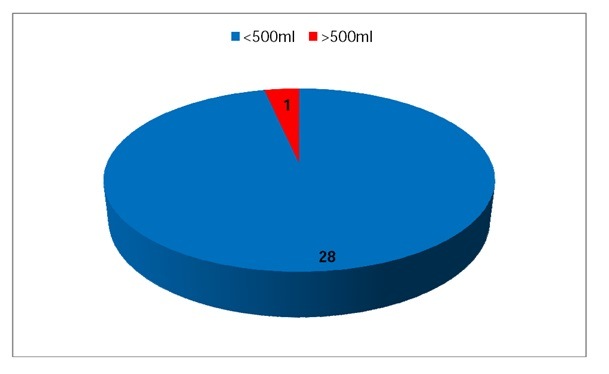
Figure 3. Average amount of blood loss (210 ml); for one among the 29 patients: 550 ml.
c. Number of artificial delivery of the placenta
Many practitioners feared to promote retained placenta by injecting oxytocin in order to enhance uterine retraction. According to the Cochrane Collaboration, there is no increase of retained placenta in patients who have received oxytocin. Similarly, in this small study, no retained placenta was found in the 29 patients who benefited from the acupunctural method.
This study showed that acupuncture is beneficial on the delivery of the placenta. The results must be confirmed in a randomized controlled trial with a larger number of participants. If the upcoming clinical trial is based on OPC concept, an update of the latest data of the Cochrane Collaboration in 2013 [20] and 2015 [21] is needed.
Discussion
An approach based on the OPC methodology may represent an acceptable and scientifically valid alternative to determine the efficacy of Acupuncture. OPC may be considered when disease natural history of the disease is well known, patient population well described, in case of extensive experience with the acupuncture treatment, stable and well known standard of care, no significant new questions of safety and effectiveness, and expectation of significant positive treatment effect.
It may be appropriate to use OPC when standard of care therapy is well established, great deal is known about the natural history of the disease, underlying patient population is well described and stable (not much variability), extensive clinical history and experience with treatment type are known, and no apparent new concerns regarding effectiveness.
Consensus among clinical communities and expectation of significantly positive treatment effect are required too.
Advantages of OPC
The OPC use offers several advantages over randomized clinical trials: smaller sample size surrogate for control group (as compared to RCT), standardized comparator for future trials, reduced cost, shortened time to completion, simpler logistic, saving time and money.
Minimum requirements
However the determination of an OPC is not a simple task. It requires rigorous and scientifically valid methodologies. An OPC should be established by a multidisciplinary team of Traditional Chinese Medicine (TCM) practitioners, and Occidental physicians in cooperation with statisticians.
A detailed analysis of publications in peer-review journals provides a threshold value (OPC), a sort of consensus on the efficacy rate of allopathic treatments currently recognized, and should be followed by a detailed analysis on how it was derived in a peer-review journal. Collaboration with a statistician can determine the adequate sample size for the clinical trial to show whether the efficacy of acupuncture is higher, lower or equal to the allopathic treatment.
An OPC must reflect the current level of care and must be periodically re-evaluated.
It is necessary for TCM practitioners to participate in TCM consensus conferences to determine OPC for each disease or symptom, in conjunction with allopathic medical practitioners and/or published results in current Western medicine practice.
Limitations of OPC
Using OPC does not mean standards can be relaxed. The trial must be well designed: intensive resource to develop the OPC, problems on agreeing to the final OPC value.
- OPC may inherit all problems seen with historical controls.
Valid historical control requires: a recent study with the same treatment; same eligibility criteria, workup, and evaluations; prognostic factors completely known and are the same in both treatment groups; no unexplained factors leading one to expect different results.
OPC needs for periodic/constant review and update. It is necessary to reassess its value after each relevant trial. OPC must reflect contemporary medical practice (temporal bias).
- OPC may inherit all the problems associated with non-concurrent control: severe and unknown selection bias; significant challenge with missing data; problems with validity of data and analysis.
Close attention must be paid to inclusion/exclusion criteria (assumption of identical populations: group of patients with same condition, demographics, and prognostic values).
Sham acupuncture
It is difficult to interpret the effects of sham needling and the extent to which such approaches can be used as valid controls in clinical trials. It has been shown that slight touch of the skin stimulates mechanoreceptors coupled to slow conducting unmyelinated (C) afferents, inducing a “limbic touch”' response resulting in emotional and hormonal reactions [23].
Sham acupuncture interventions are often associated with moderate nonspecific effects.
RCT‘s. Comparing real acupuncture with sham acupuncture presents small power. According to Linde et al. [24], the differentiation between specific effects of acupuncture and non-specific effects (placebo) required the recruitment of 800 subjects in a double-blind randomized controlled trial in order to obtain a power of 80%, and a standardized mean difference (SMD) 0.2 for a specific outcome measure.
OPC concept has the advantage of not using minimal, superficial, sham, or “placebo” acupuncture for the control group.
Conclusion
Challenges remain in the process to demonstrate the efficacy of acupuncture, despite the emergence of evidence-based medicine [25]. A more applicable and innovative research methodology that can reflect the effectiveness of acupuncture is needed, for improving future research into this integrative intervention, and CT’s based on OPC concept are worth developing.
To date, the gold standard for evaluation of a treatment is RCT with high methodological quality and high power, which can provides the highest level of scientific evidence. It would be interesting to add OPC methodology in the recommendations of grades, especially when blinding is difficult. A combined approach using a multidisciplinary team incorporating considerations of efficacy, effectiveness and qualitative measures, will strengthen the evidence base for acupuncture [26].
The OPC is a criteria based on published literature (meta-analyzes) and/or reliable registries OPC may be considered when disease natural history is well known, patient population well described, in case of extensive experience with acupuncture treatment, stable and well known standard of care, no significant new questions of safety and effectiveness, and expectation of significant positive treatment effect. The OPC use offers several advantages over randomized clinical trials: smaller sample size, standardized comparator for future trials, reduced cost, shortened time to completion, simpler logistic.
However the determination of an OPC is not a simple task. It requires rigorous and scientifically valid methodologies. An OPC should be established by a multidisciplinary team of Traditional Chinese Medicine (TCM) practitioners, and Western physicians in cooperation with statisticians.
OPC concept could represent an acceptable and scientifically valid alternative to determine effectiveness of acupuncture. Acupuncturists should consider this methodology when randomization and double-blindness are problematic.
Abbreviations
CAM: complementary and alternative medicine
CI: confidence interval
CT: clinical trial
FDA: Food and Drug Administration
ICMART: International Council of Medical Acupuncture and Related Technique
OB: obstetric
OPC: objective performance criteria
RCT: randomized control trial
RR: relative risk
SMD: standardized mean difference
TCM: Traditional Chinese Medicine
US: the United States
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
· Anne-Sophie Piau, Sophie Broquet (Jeanne de Flandre Hospital, Lille, France): investigators of the trial on perineal relaxation during fetal expulsion.
· Caroline Mollet, Sandra Dumortier (Paul Gellé Hospital Maternity, Roubaix, France): investigators of the trial on the third stage of labor.
· Prof Véronique Houfflin-Debarge, Hélène Montaigne, MD: Lille 2 University, France.
Références
1. Sapirstein W. The conduct of clinical trials: a Food and Drug Agency perspective. ASAIO J. 2000;46(1):29-30. PubMed
2. Faris O, Chen E, Berman M, Moynahan M, Zuckerman B. A US Food and Drug Administration perspective on cardiac resynchronization and ventricular assist device trials. Congest Heart Fail. 2005;11(4):207-211. PubMed
3. Dorrothy B. Standardized Objective Performance Criteria and Control Datasets - How the FDA is working to determine the potential role for these criteria in peripheral device regulation, and how they are best established. (April 2006): Available from URL: http://bmctoday.net/evtoday/2006/04/article.asp?f=EVT0406_FDA.html
4. Chen E, Sapirstein W, Ahn C, Swain J, Zuckermn B. FDA Perspective on Clinical Trial Design for Cardiovascular Devices. Ann Thorac Surg., 2006;82:773-5. PubMed
5 Grunkemeier GL, Ji R, Starr A. Prosthetic heart valves: Objective Performance Criteria versus randomized clinical trial. Ann Thorac Surg. 2006;82(3):776-780. PubMed
6. Conte MS, Geraghty PJ, Bradbury AW, Hevelone ND, Lipsitz SR, Moneta GL, Nehler MR, Powell RJ, Sidawy AN. Suggested objective performance goals and clinical trial design for evaluating catheter-based treatment of critical limb ischemia. J Vasc Surg. 2009;50(6):1462-73. PubMed
7. Kumar A, Brooks SS, Cavanaugh K, Zuckerman B. FDA perspective on objective performance goals and clinical trial design for evaluating catheter-based treatment of critical limb ischemia. J Vasc Surg. 2009 Dec;50(6):1474-76. PubMed
8. Parides MK, Moskowitz AJ, Ascheim DD, Rose EA, Gelijns AC. Progress versus precision challenges in clinical trial design for left ventricular assist devices, Ann Thorac Surg. 2006;82:1140-46. PubMed
9. Rocha-Singh KJ, Jaff MR, Cratree TR, Bloch DA, Ansel G, VIVA Physicians, Inc. Performance goals and endpoint assessments for clinical trials of femoropopliteal bare nitinol stents in patients with symptomatic peripheral arterial disease. Catheter Cardiovasc Interv. 2007;69(6):910-9. PubMed
10. Brignol TN, Verta P. Can OPC (Objective Performance Criteria) used in FDA approval for medical devices represent an acceptable and scientifically valid alternative to show efficacy in clinical trials in Acupuncture? XIII ICMART World Congress on Medical Acupuncture – The Hague (Netherland). 13-15 May 2011. Abstract 22 (p 31). Available from URL: http://www.icmart.org/files/icmart_congress_2011_abstract.pdf
11. Brignol TN, Verta P. Une méthodologie basée sur l’OPC (Objective performance criteria) est-elle valable pour prouver l’efficacité de l’acupuncture ? Acupuncture & Moxibustion, 2011;10(3): 204-206. Available from URL: https://www.meridiens.org/mrd/IMG/pdf/Acupuncture_et_Moxibustion__Brignol-Verta_vol10_no3_2011.pdf
12. Mårtensson L, Kvist L, Hermansson E. A national survey of how acupuncture is currently used in midwifery care at Swedish maternity units. Midwifery. 2011;27(1):87-92. PubMed
13. Münstedt K, Thienel J, Hrogovic I, Hackethal A, Kalder M, Misselwitz B. Use of acupuncture and other CAM methods in obstetrics: an analysis of 409,413 deliveries from Hesse, Germany. J Altern Complement Med. 2011;17(5):421-26. PubMed
14. Stéphan JM. DIU d’Acupuncture Obstétricale : tableaux d’une exposition, Acupuncture & Moxibustion, 2013;12(2): 147-151. Available from URL: https://www.meridiens.org/acuMoxi/douzedeux/STEPHAN-DIU_perinee.pdf.
15. Stéphan JM. DIU d’Acupuncture Obstétricale : tableaux d’une exposition. Délivrance et cholestase gravidique. Acupuncture & Moxibustion. 2014;13(3):213-217. Available from URL: https://www.meridiens.org/acuMoxi/treizetrois/STEPHAN-DIU13-3.pdf.
16. Gouan L, Yiliang Z. Clinical report about controlling postpartum hemorrhage with electric stimulation at acupuncture points. in selections from article abstracts on acupuncture and moxibustion, Beijing 1987:134.
17. Xu L, Liang-fang S, Jun-yan L, Wei-hong Z. Needling Hegu to accelerate the second labor stage, International Journal of Clinical Acupuncture. 1995;6(1):101-103.
18. Bader W, Ast S, Hatzmann W. Die Bedeutung der Akupunktur in der Plazentarperiode. Dt. Ztschr. f. Akupunktur. 2000;4:264-268.
19. http://www.ncbi.nlm.nih.gov/pubmed/25238645Cotter AM, Ness A, Tolosa JE. Prophylactic oxytocin for the third stage of labour. Cochrane Database Syst Rev 2001;4:CD001808. PubMed
20. Westhoff G, Cotter AM, Tolosa JE. Prophylactic oxytocin for the third stage of labour to prevent postpartum haemorrhage. Cochrane Database Syst Rev. 2013 Oct 30;10:CD001808.
21. Begley CM, Gyte GM, Devane D, McGuire W, Weeks A. Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2015 Mar 2;3:CD007412. doi: 10.1002/14651858.CD007412.pub4. PubMed
22. Benedetti F, Maggi G, Lopiano L et al. Open versus hidden medical treatments: the patient’s knowledge about a therapy affects the therapy outcome. Prev Treat. 2003; doi: 10.1037/1522-3736.6.1.61a.
23. Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med. 2006;24(1):13-5. PubMed
24. Linde K, Niemann K, Schneider A, Meissner K. How large are the nonspecific effects of acupuncture? A meta-analysis of randomized controlled trials. BMC Med. 2010;8:75. PubMed
25. Godwin J. Rising to the challenges of evidence-based medicine: a way forward for acupuncture. J Altern Comlement Med. 2014 Nov;20(11):805-9. doi: 10.1089/acm.2014.0213. Epub 2014 Sep 19. PubMed
26. Langevin HM, Wayne PM, Macpherson H, Schnyer R, Milley RM, Napadow V, Lao L, Park J, Harris RE, Cohen M, Sherman KJ, Haramati A, Hammerschlag R. Paradoxes in acupuncture research: strategies for moving forward. Evid Based Complement Alternat Med. 2011;2011:180805. doi: 10.1155/2011/180805. Epub 2010 Oct 11. PubMed
To cite: Brignol TN, Stéphan JM, Verta A. Acupuncture clinical trials without a control group in Obstetrics : a French experience alternative approach using OPC (objective performance criteria). Acupuncture & Moxibustion (online). Feb 2016. Available from: URL: https://meridiens.org/acuMoxi/Quinzeun/Brignol_OPC.pdf